Facial dystonias
is a disease which causes significant disability to the patient as it
progresses over time. The time tested and most reliable therapy for hemifacial
and blepharospasm is repeated botulinum toxin (Botox, Allergan) injection given
subcutaneously. It is also very effective in the reduction of deep creases and
wrinkles formed by weakening of the facial muscles with age1. The
treatment requires injection of botulinum
toxin just beneath the skin so that it can diffuse to the targeted facial
muscles. Although the injection is given with a 30 gauge needle the patients
can feel varying degree of pain and anxiety while receiving this treatment in
the very sensitive periocular region2. An effective alternate method
to avoid this pain and discomfort is by using eutectic mixture of local
anaesthetics.
EMLA cream
is available as an emulsion which is a eutectic mixture containing 2.5% prilocaine and 2.5% lidocaine established to numb the skin
surface. Both the drugs which anesthetise the skin have been mixed in such a
way that the cream does not melt at room temperature and the ingredients are
present as liquid oil instead of crystals. Indications of EMLA cream include
topical pain relief for needle pricks, especially in children, and minor
surgery involving superficial skin. The
depth of anaesthesia is proportional to the duration of application of the
cream on the skin. Skin is anesthetised 1-2 mm after 60 minutes of application
while after 3-4 hours the depth of anaesthesia increases to 6 mm3,4.
For minor surgical procedures involving needle
insertion the recommended concentration of EMLA cream is the most effective and
safe agent which can anesthetise the skin5 (including blood testing,
intravenous cannulation, lumbar puncture and botulinum A toxin injections). It
is also very useful for minor procedures used in dermatology such as removal of
warts, biopsy of skin and laser treatment6. Adequate anaesthesia of skin is
attained after the cream has been applied for 1 hour. It reaches its peak in
2-3 hours and remains present for 1-2 hours after the cream has been removed.
The rationale of our study was to find an effective drug to relieve pain
in patients receiving Botulinum toxin injections for the treatment of facial
dystonias. Review of literature shows studies on this topic but no local
literature was found. The purpose of the study was to determine the usefulness
of EMLA cream (Eutectic Mixture of Local Anesthetics) in pain reduction while
injecting botulinum toxin in patients with hemifacial spasm and blepharospasm.
MATERIAL
& METHODS
The study was conducted at Yaqin Vision Center, Lahore from Jan
2015 to Dec 2018 as a Quasi experimental study. Ethical Approval of the study
was taken from the Ethical review committee of Lahore General Hospital, Lahore.
Patients included in the study were > 25 years of age of both genders who
presented with hemifacial spasm and essential blepharospasm. Only those
patients were selected who had already undergone botulinum toxin A injection
(Botox, Allergan) without use of EMLA cream previously, as it was not readily
available before. Patients who were excluded from the study had blepharospasm
due to secondary reasons such as drugs, ophthalmic and neurological conditions.
Intracranial pathology was ruled out in all patients before start of treatment
using Computed tomography or Magnetic resonance imaging.
Patients undergoing routine treatment of Blepharospasm and
Hemifacial spasm since 2010 were offered pre-injection EMLA cream application
to reduce the pain during injections. The sample
size (n) was calculated by 95%
confidence level, with anticipated population proportion (P) 74% and keeping
absolute precision (d) 10%. A total of 74 Botulinum A toxin injections
were given for routine treatment of blepharospam and
hemifacial spasm, half of which were administered without the use of any
topical analgesia while other half were offered EMLA cream treatment prior to
injection. The cream was applied for 15 minutes before the procedure. Each
Botox injection was carefully administrated in the area where EMLA cream was
applied. We used Botulinum Toxin-A 100 Units (Botox, Allergan) diluted in 2 ml
normal saline. The injections were given using a 1 ml insulin syringe, with a
30G needle (microlance 30G × ¾ 0.4 × 19
mm).
Pain was
assessed as mild, moderate and severe without and later with EMLA cream
application by the consultant administering the medication. Pain grading was
modified from the Visual Analog Scale which is a reliable tool used worldwide7.
Data entry and analysis was done using SPSS Statistics for
Windows package, version 25.0 (IBM, USA). Categorical variables such as pain
scoring was analysed using the chi square test. The study reported on the
effects of EMLA with regard to the mean difference in pain between the group
that received EMLA for Botox injection and the control group with no
intervention previously.
RESULTS
Among 37 cases of facial dystonias, 17 (45.9%) were males
and 20 (54.1%) were females with a male to female ratio of 1:1.8 (Table 1).
Table 1: Comparison of gender distribution between groups.
|
Gender |
Use of EMLA |
Total |
|
|
Not Used |
Used |
||
|
Male |
17 |
17 |
34 |
|
45.9% |
45.9% |
45.9% |
|
|
Female |
20 |
20 |
40 |
|
54.1% |
54.1% |
54.1% |
|
|
Total |
37 |
37 |
74 |
|
100.0% |
100.0% |
100.0% |
|
Categorizing the patients into three age groups revealed
that majority of the patients 81.1% (60 patients) were above 45 years of age
(Table 2).
Table 2: Comparison of age groups distribution between groups.
|
Age Groups |
Use of EMLA |
Total |
|
|
Not Used |
Used |
||
|
19-30 years |
4 |
4 |
8 |
|
10.8% |
10.8% |
10.8% |
|
|
31-45 years |
3 |
3 |
6 |
|
8.1% |
8.1% |
8.1% |
|
|
>45 years |
30 |
30 |
60 |
|
81.1% |
81.1% |
81.1% |
|
|
Total |
37 |
37 |
74 |
|
100.0% |
100.0% |
100.0% |
|
Blepharospasm was present in 46 patients (62.2 %) and 28
patients (37.8%) were diagnosed with Hemifacial spasm (Table-3).
Table
3: Comparison of diagnosis
between groups.
|
Diagnosis |
Use of EMLA |
Total |
|
|
Not Used |
Used |
||
|
Blepharospasm |
23 |
23 |
46 |
|
62.2% |
62.2% |
62.2% |
|
|
Hemifacial Spasm |
14 |
14 |
28 |
|
37.8% |
37.8% |
37.8% |
|
|
Total |
37 |
37 |
74 |
|
100.0% |
100.0% |
100.0% |
|
Patients were categorized in three groups according to pain:
mild pain, moderate pain and severe pain. It was seen that in patients in which
EMLA was not used, 21.6% (8 patients) had severe pain, 45.9% (17) had moderate
pain, and 32.4% (12) had mild pain. However EMLA cream was used 89.2% (33)
patients had mild pain, 8.1% (3 patients) had moderate pain and only 2.7% (only
1 patient) had severe pain. (Table 4). This demonstrates a significant
reduction in pain during the procedure with use of topical EMLA cream (Figure 1).
Table
4: Comparison of pain scale
between groups.
|
Pain Scale |
Use of EMLA |
Total |
p-value |
|
|
Not Used |
Used |
|||
|
Mild Pain |
12 |
33 |
45 |
0.000004 |
|
32.4% |
89.2% |
60.8% |
||
|
Moderate Pain |
17 |
3 |
20 |
|
|
45.9% |
8.1% |
27.0% |
||
|
Severe Pain |
8 |
1 |
9 |
|
|
21.6% |
2.7% |
12.2% |
||
|
Total |
37 |
37 |
74 |
|
|
100.0% |
100.0% |
100.0% |
||
*A small p-value
(typically ≤ 0.05) indicates strongest evidence of results being
significant.
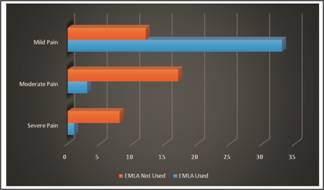
Fig. 1: Comparison
of pain with and without the use of EMLA cream.
The effectiveness of the Botox injections among these
patients was also noted on follow up by categorizing them into 3 groups: No
effect, Fair effect and Good effect. It was seen that there was no significant
difference in results and effectiveness of Botulinum toxin A injections on
facial dystonias among patients with EMLA, and without use of topical EMLA cream
(Table 5).
Table
5: Comparison of effect of
Botox on spasm.
|
Effect of Botox on Spasm |
Use of EMLA |
Total |
p-value |
|
|
Not Used |
Used |
|||
|
No Effect |
5 |
5 |
10 |
0.356 |
|
13.5% |
13.5% |
13.5% |
||
|
Fair Effect of Botox |
2 |
0 |
2 |
|
|
5.4% |
0.0% |
2.7% |
||
|
Good effect of Botox |
30 |
32 |
62 |
|
|
81.1% |
86.5% |
83.8% |
||
|
Total |
37 |
37 |
74 |
|
|
100.0% |
100.0% |
100.0% |
||
DISCUSSION
Topical anaesthetics are commonly used for routine minor procedures like
subcutaneous injections, intravenous cannulisation, catheterization and removal
of superficial skin lesions. EMLA has been
shown to be tolerated well by the patients. In our study no patients
experienced any side effect. Small sample size and experienced injector could
be the reason for this. EMLA cream has not been found to show any toxicity
except in infants. Local side effects which have been reported by other
physicians include contact dermatitis, erythema, oedema and increased pigmentation
of the skin8. One case report has shown that respiratory depression
and seizures can occur. The worst
complication reported was Methaemoglobinaemia which can be potentially fatal but
only infants develop this condition9,10.
Soylev MF et al11 demonstrated that percutaneous anaesthesia produced
by using EMLA cream is quite adequate and it is a safe technique to enhance the
patient comfort when repeated botulinum toxin injections are required for
facial dyskinesia. Applying a
dot of EMLA cream is easy, convenient, and inexpensive way of anesthetizing the
site of injection.
Many other methods of lowering pain in Botox
injections are suggested. Using a small gauge needle as demonstrated by Flynn TC et al12, is an obviously a preferred intervention, combined
with a minimal number of pricks, also helps ensure proper management of
discomfort. Using an isotonic mixing solution (preservative-containing
saline solution) for reconstitution of the drug and reducing the temperature of
the skin with the use of various cooling techniques (eg, ice, aerosol sprays) have
also been reported to reduce injection discomfort in a study done by Alam M et
al13. Same results were obtained by Linder JS et al14, by
using various skin cooling techniques. However, Kuwahara RT et al15
reported that cold sponging with ice, is inconvenient and the pain control it
affords is only partially effective. Essential blepharospasm is an involuntary
spasm of eyelid muscles affecting patients in fifth and sixth decade of life
and predominantly affect females than male with 3:116. Hemifacial spasm is a neuromuscular movement disorder
characterized by brief or persistent involuntary contractions of the muscles
innervated by the facial nerve17.
Botox injections are effective treatment for both these facial dystonias i.e.
for blepharospasm as shown by Hellman A
et al18 in a recent study, and also for hemifacial spasm as demonstrated
by Singh S et al19 with a success rate of 95%. Botulinum A toxin
inhibits cholinergic transmission at neuromuscular synapses and relaxes
muscles. Clinical effects are usually observed after 2–5 days and last for
16–24 weeks as reported by Basaret al20.
The pain during this procedure can be measured by a standardized system or
scale, like Visual Analogue Scale (VAS), that we modified for reliable measurement
of pain and its relief21.
In our study, we applied Botulinum toxin A (Botox) injections in
74 eyes, among 34 (45.9%) males and 40 (54.1%) females. Among these patients 46
(62.2%) presented with blepharospasm and 28 (37.8%) had hemifacial spasm.
We grouped the patients according to pain suffered, into three
categories: mild pain, moderate pain and severe pain. It was seen that in 89.2%
(33) patients in which EMLA was used had only mild pain, 8.1% (3 patients) had
moderate pain and 2.7% (only 1 patient) had severe pain. However, among the
patients in which EMLA was not used, 21.6% (8 patients) had severe pain, 45.9% (17
patients) had moderate pain, and 32.4% (12 patients) had mild pain. All these
results clearly indicated that topical EMLA cream can be used as an effective
tool in management of pain among patients having Botox injections for their
facial dystonia treatments. Similar results were seen in a comprehensive study
done on anaesthetic effectiveness of EMLA cream during Botulinum A injections
in eyelids by Soylev MF et al11.
Another recent study by Elibol Oet al22 reported that EMLA
applications significantly decrease the pain associated with periocular
botulinum toxin injections. It also demonstrated that patients had a slight
preference for EMLA cream over skin cooling for pain relief. In a study done by
Barry L. Eppley, MD23 on
twenty patients, receiving 200 Botox injections in the glabellar area, it was
seen that patients experienced a 60% reduction in pain in EMLA pre-treated
sites compared with that in matched control sites. Similar dose of botulinum
toxin can usually be repeated to get stable results of the injection24.
The use of EMLA, however, did not have any
significant effect on efficacy of botulinum injection in relieving the spasm
itself, apart from reduction in pain.
The limitation of our study was the limited
number of patients in our study. Moreover it was also performed at a single
centre. A multi-centre study is needed to find the efficacy in large sample of
population.
CONCLUSION
Use of EMLA cream can dramatically reduce pain, make
administration of botulinum toxin A injection easier in patients with blepharospasm
and hemifacial spasm. This can improve the therapeutic relationship of the patients with health professionals.
Disclosure
The authors have no financial benefit or conflicts of interest in this
work.
Author’s Affiliation
Prof. Muhammad Moin
MBBS, MRCOphth, FRCS, FRCOphth
Department of Ophthalmology,
Postgraduate Medical Institute,
Lahore General Hospital,
Yaqin Vision Eye Center,
Lahore.
Abdullah Irfan
PG Trainee Ophthalmology,
Lahore General Hospital,
Lahore.
Author’s
Contribution
Prof. Muhammad Moin
Data Collection, Study Design, Critical Analysis.
Abdullah Irfan
Manuscript writing, Statistical Analysis.
REFERENCES
1. Beer KR, Wilson F. Skin cooling provides minimal relief of patient discomfort
during periocular botulinum toxin type A injection. Dermatol Surg. 2011; 37 (6):
870-2.
2. Yazuver R, Demirtas Y. Painful injections with botox. Plast Reconstructive Surg.
2003; 111: 509-510.
3. Friedman PM, Mafong EA, Friedman ES, Geronemus RG. Topical anesthetics update: EMLA and
beyond. Dermatol Surg. 2001; 27: 1019-1026.
4. Wahlgreen CF, Quiding H. Depth of
cutaneous analgesia after application of a eutectic mixture of the local
anestheticslidocaine and prilocaine (EMLA cream). J Am Acad Dermatol. 2000;
42: 584-588.
5. Russell SC, Doyle E. A risk-benefit assessment of topical
percutaneous local anaesthetics in children. Drug Saf. 1997; 16 (4): 279-87.
6. McCafferty DF, Woolfson AD, Handley J, et al. Effect of
percutaneous local anaesthetics on pain reduction during pulse dye treatment of
portwine stains. Br J Anaesthesia, 1997; 78: 286-9.
7. Dauphin AP, Guillemin F, Virion
JM, Briançon
S. Bias and Precision in Visual Analogue Scales: A Randomized
Controlled Trial. American Journal of Epidemiology, 1999; 150 (10): 1117-1127.
8. Godwin Y, Brotherston M.
Hyperpigmentation following the use of EMLA cream. Br J Plast Surg. 2001; 54 (1):
82-83.
9. Rincon E, Baker RL, Iglesias AJ, et al.
CNS toxicity after topical application of EMLA cream on a toddler with
molluscumcontagiosum. Pediatr Emerg Care, 2000; 16 (4): 252-254.
10. Essink-Tebbes
CM, Wuis EW, Liem KD, et al. Safety of lidocaine-prilocaine cream application four times a day
in premature neonates: A pilot study. Eur J Pediatr. 1999; 158 (5): 421-423.
11. Soylev MF, Kocak
N, Kuvaki B, Ozkan SB, Kir E. Anesthesia with EMLA cream for botulinum A toxin injection
into eyelids. Ophthalmologica. 2002; 216: 355-358.
12. Flynn TC, Carruthers A, Carruthers J.
Surgical pearl: the use of the Ultra-Fine II short needle 0.3-cc insulin
syringe for botulinum toxin injections. J Am Acad Dermatol. 2002; 46: 931-932.
13. Alam M, Dover JS, Arndt KA. Pain
associated with injection of botulinum A exotoxin reconstituted using isotonic
sodium chloride with and without preservative: a double-blind randomized
controlled trial. Arch Dermatol. 2002; 138: 510-514.
14. Linder JS, Edmonson BC, Laquis SJ, Drewry
RD Jr, Fleming JC. Skin cooling before periocular botulinum toxin A
injection. Ophthal Plast Reconstr Surg. 2002; 18: 441-442.
15. Kuwahara RT, Skinner RB. EMLA versus
ice as a topical anesthetic. Dermatol Surg. 2001; 27: 495.
16. Jankovic
J, Orman J. Blepharospasm:
Demographic and clinical survey of 250 patients. Annals of ophthalmology, 16
(4): 371-6. May 1984.
17. Rosenstengel
C, Matthes M, Baldauf J, Fleck S, Schroeder H. Hemifacial spasm: conservative and surgical treatment
options. Dtsch Arztebl Int. 2012; 109 (41): 667–673.
18. Hellman A, Torres-Russotto D. Botulinum toxin in the management of
blepharospasm: current evidence and recent developments. Ther Adv Neurol Disord.
2015; 8 (2): 82-91.
19. Singh S. Botulinum toxin in hemifacial spasm:
Revisited. Indian J Plast Surg. 2013; 46 (1): 159-160.
20. Basar E, Arici C. Use of Botulinum neurotoxin in
ophthalmology. Turk J Ophthalmol. 2016; 46 (6): 282-290.
21. Sherman SA, Eisen S, Burwinkle TM, Varni
JW. The Peds QL Present Functioning Visual Analogue Scales: preliminary
reliability and validity. Health Qual Life Outcomes, 2006; 4: 75.
22. Elibol O,
Ozkan B,
Hekimhan PK,
Cağlar Y. Efficacy of skin cooling and EMLA cream application for pain
relief of periocular botulinum toxin injection. Ophthalmic
Plast Reconstr Surg. 2007 Mar-Apr; 23 (2): 130-3.
23. Barry L. Eppley,
MD. Easing
Botox Administration with EMLA Cream. Aesthetic Surg J. 2004; 24: 79-81.
24. Moin M, Khalid S. Fixed dose botulinum
toxin therapy for Blepharospasm. Pak J Ophthal. 2016; 32 (2): 91-94.